Benefits of Gastric Bypass Surgery for Obesity Management in Diabetics
Brian Chin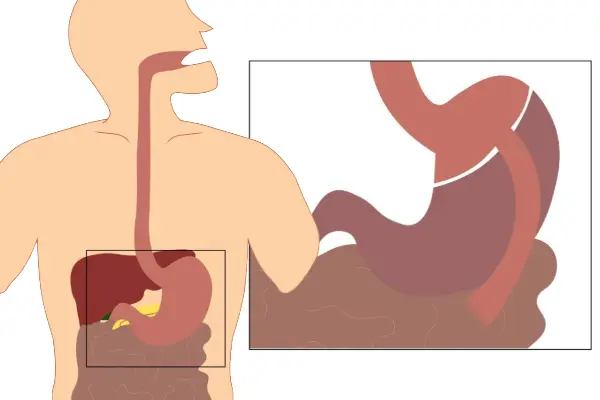
Managing obesity and diabetes together can feel overwhelming. Many patients try countless diets and exercise plans, only to fall into a frustrating cycle of losing and regaining weight. For those with Type 2 diabetes, this struggle is even more challenging. Fortunately, gastric bypass surgery has emerged as one of the most effective tools for both weight loss and diabetes management.
What Is Gastric Bypass Surgery?
The Roux-en-Y gastric bypass (RYGB) is one of the most widely performed bariatric procedures. During surgery, the stomach is divided into two sections:
- A small pouch that becomes the new stomach and can only hold a small amount of food.
- A larger gastric remnant that no longer directly receives food but still produces important digestive juices.
The surgeon also reroutes the small intestine so food passes directly from the pouch into the intestine, bypassing much of the stomach. This change not only restricts food intake but also alters nutrient absorption and hormonal responses that regulate appetite and metabolism.
Key Benefits of Gastric Bypass for Diabetics
1. Remission of Type 2 Diabetes
One of the most remarkable outcomes is diabetes remission rates of up to 80%. What’s surprising is that this often occurs before significant weight loss happens. After surgery, blood sugar levels frequently normalize within days, reducing or even eliminating the need for diabetes medications.
2. Positive Hormonal Changes
Gastric bypass triggers beneficial hormonal shifts. For example, levels of GLP-1 (glucagon-like peptide-1) increase after surgery. GLP-1 stimulates insulin secretion, suppresses glucagon (which raises blood sugar), and helps patients feel fuller faster. These changes play a direct role in improving diabetes outcomes.
3. Improvements in Related Health Conditions
Diabetes rarely comes alone. Many patients also face high blood pressure, high cholesterol, sleep apnea, and abnormal triglyceride levels. Studies show that gastric bypass surgery can lead to significant improvement—or complete resolution—of these obesity-related conditions.
4. Sustained Weight Loss
Patients typically lose 60–80% of their excess body weight after gastric bypass. This weight reduction not only improves diabetes but also enhances overall health, mobility, and quality of life. For many, this marks the end of years of failed dieting and yo-yo weight loss.
5. Emotional and Lifestyle Benefits
The benefits aren’t just physical. Weight loss surgery often leads to boosted self-confidence, emotional well-being, and the ability to participate in activities that were once limited by obesity. Patients frequently report feeling like they’ve regained control of their lives.
Important Considerations
While gastric bypass is highly effective, it’s not a quick fix. Long-term success depends on lifestyle changes, nutritional supplements, and ongoing medical follow-up. Patients must commit to healthy eating, regular physical activity, and regular monitoring to maintain results and avoid complications such as nutrient deficiencies.
Is Gastric Bypass Right for You?
If you are living with obesity and Type 2 diabetes, gastric bypass surgery may offer a life-changing solution. At BASS Bariatric Surgery Center, our expert surgeons—Dr. Brian Chin and Dr. Jason Moy—have helped countless patients achieve diabetes remission and sustainable weight loss.
Call us today at (925) 940-1052 or request a consultation online to explore whether gastric bypass surgery is right for you.
FAQs About Gastric Bypass and Diabetes
Does gastric bypass cure diabetes permanently?
Not always. Many patients achieve remission, but long-term results depend on individual health, lifestyle, and follow-up care.
How soon after gastric bypass will diabetes improve?
Blood sugar levels often improve within days, even before major weight loss occurs.
Is gastric bypass safe for diabetics?
Yes, when performed by experienced bariatric surgeons. Risks exist but are far outweighed by the long-term benefits for many patients.
.webp)

.webp)