Can Bariatric Surgery Help Treat or Reverse Type 2 Diabetes?
Brian Chin.webp)
Are you or someone you know living with both obesity and type 2 diabetes? You’re not alone. More than 37 million Americans have diabetes, and over 90% of cases are linked to being overweight or obese. For many, diet, exercise, and medications can help, but they don’t always provide lasting results.
That’s why bariatric surgery has become a life-changing option — not just for weight loss, but also for improving or even achieving remission of type 2 diabetes. In this guide, we’ll explain the strong connection between obesity and diabetes, how bariatric surgery works to improve blood sugar control, and what patients can realistically expect.
Understanding the Link Between Obesity and Type 2 Diabetes
Type 2 diabetes is a chronic condition where the body becomes resistant to insulin, the hormone that helps move sugar (glucose) from your blood into your cells for energy. When insulin can’t do its job effectively, glucose builds up in the bloodstream, leading to high blood sugar levels.
Obesity is one of the biggest risk factors for developing type 2 diabetes. Extra body fat, especially around the abdomen, creates inflammation and hormonal changes that make the body more resistant to insulin. Over time, this resistance can push blood sugar levels higher and higher.
- According to the CDC, more than 9 in 10 people with type 2 diabetes are overweight or obese.
- Being obese can increase the risk of developing type 2 diabetes sevenfold compared to someone at a healthy weight.
This connection explains why a procedure designed to support major weight loss can also lead to dramatic improvements in diabetes.
How Bariatric Surgery Improves Diabetes
Bariatric surgery isn’t just about eating less food — it also changes the way your body processes food and regulates blood sugar. Here are some of the key ways it helps:
- Improved Insulin Sensitivity
Many patients notice better blood sugar control within days of surgery, often before significant weight loss occurs. That’s because bariatric procedures trigger powerful hormonal changes that make the body more responsive to insulin. - Lower Ghrelin, Higher Satiety
Surgeries like gastric sleeve reduce the stomach’s ability to produce ghrelin, the hunger hormone. Less ghrelin means reduced appetite and improved portion control. - Changes in the Gut Microbiome
After surgery, the gut bacteria that influence metabolism shift in a healthier direction. This helps regulate how the body processes glucose and fat. - Reduced Inflammation
Obesity drives chronic inflammation, which worsens insulin resistance. Weight loss combined with metabolic changes from surgery helps lower this inflammation.
Because of these combined effects, bariatric surgery is sometimes called “metabolic surgery” — it doesn’t just reduce weight, it helps reset the body’s metabolism.
Is Bariatric Surgery a Long-Term Solution for Diabetes?
Many studies have found that 30% to 80% of patients with type 2 diabetes experience remission after bariatric surgery. Remission means blood sugar levels return to normal without the need for diabetes medication.
However, it’s important to set realistic expectations:
- Remission rates vary depending on how long you’ve had diabetes and how severe it is before surgery. Patients who undergo surgery earlier in their diagnosis tend to have better outcomes.
- The type of surgery matters. Gastric bypass and duodenal switch generally show the highest remission rates, while gastric sleeve also produces excellent results for many patients.
- Lifestyle still matters. Bariatric surgery is not a “cure.” Long-term success requires permanent lifestyle changes including balanced nutrition, regular physical activity, and follow-up care.
Even for patients who don’t achieve complete remission, bariatric surgery almost always improves blood sugar control and reduces the need for medications. Many patients also see improvements in related conditions like high blood pressure, sleep apnea, and high cholesterol.
Which Bariatric Surgery Options Are Best for Diabetes?
At BASS Bariatric Surgery Center, we provide several surgical options. Each procedure has unique benefits, and your surgeon will recommend the best one for your health profile:
- Gastric Bypass (Roux-en-Y): Creates a small stomach pouch and reroutes part of the small intestine. Proven to achieve some of the highest diabetes remission rates.
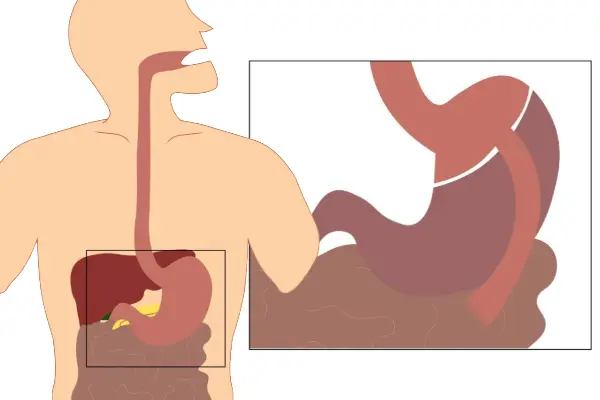
- Sleeve Gastrectomy: Removes about 80% of the stomach, reducing hunger hormones and helping patients feel full sooner. Effective for both weight loss and diabetes improvement.
- Adjustable Gastric Band: Places a band around the stomach to limit food intake. Diabetes improvements are less dramatic compared to other surgeries.
- Duodenal Switch: Combines a sleeve with significant intestinal rerouting, producing powerful weight loss and metabolic changes. Typically reserved for patients with severe obesity or diabetes.
Learn more about each procedure: Gastric Sleeve, Gastric Bypass, Gastric Band, Duodenal Switch.
Life After Surgery: Diabetes and Beyond
After bariatric surgery, many patients notice:
- Blood sugar levels normalize within days or weeks
- Reduced or eliminated need for insulin and diabetes medications
- Improved cholesterol, blood pressure, and heart health
- Higher energy levels and reduced joint pain
- Lower long-term risk of diabetes complications, such as nerve damage or kidney disease
To maintain these benefits, patients commit to lifelong follow-up care, nutritional monitoring, and healthy lifestyle habits.
FAQs About Bariatric Surgery and Diabetes
Can bariatric surgery reverse type 2 diabetes?
Yes, many patients achieve remission, but results depend on individual factors. Even without full remission, most see significant improvement in blood sugar control.
Which bariatric surgery has the best diabetes results?
Studies show gastric bypass and duodenal switch often have the highest remission rates, but sleeve gastrectomy is also highly effective and safer for many patients.
How soon will my diabetes improve after surgery?
Many patients see improvement within days, before major weight loss occurs, thanks to hormonal changes.
Is diabetes remission permanent after weight loss surgery?
It can last for many years, but lifestyle habits, age, and disease history play a role. Ongoing medical care is essential.
Take the First Step Toward Lasting Health
If you’re struggling with both obesity and type 2 diabetes, bariatric surgery may be the tool that helps you regain control of your health. At BASS Bariatric Surgery Center, Dr. Brian Chin, Dr. Jason Moy, and our expert team have helped countless patients achieve lasting weight loss and diabetes remission.
Serving Walnut Creek, Brentwood, and the entire East Bay Area.
Call 925-940-1052 or request a consultation online.